USCOM in the Operating Theatre.
You will have seen the USCOM being used increasingly frequently in the operating theatre, particularly during major cases. Why is this so?
Let’s consider the average patient undergoing major surgery. Firstly, they may be on a host of medications for pre-existing conditions with heart disease, hypertension and diabetes being particularly prevalent. Patients may well have been given a bowel prep, which can cause significant loss of fluid from the body, as can pre-operative vomiting. Even in an elective case, the patient will have been fasted for many hours or even overnight before their operation. The anaesthetist will then use a plethora of drugs which have significant cardiovascular activity, ranging from myocardial depression to vasodilation. There may be blood loss or evaporative loss of fluid from the open abdomen, there may be antibiotics given intravenously which can have vascular activity, and as if all this wasn't enough, the anaesthetist may well use an epidural or spinal anaesthetic as well. What if the patient has pain, what will that do to their hemodynamics? Given all of the above, it is hardly surprising that major changes in the patient’s haemodynamic status occur during surgery.
Whilst the measurement of blood pressure, heart rate and pulse oximetry are routine, do these really tell us much about the true haemodynamic picture?
Let's take a look at a typical example of the haemodynamic trends in a patient undergoing left hemicolectomy.
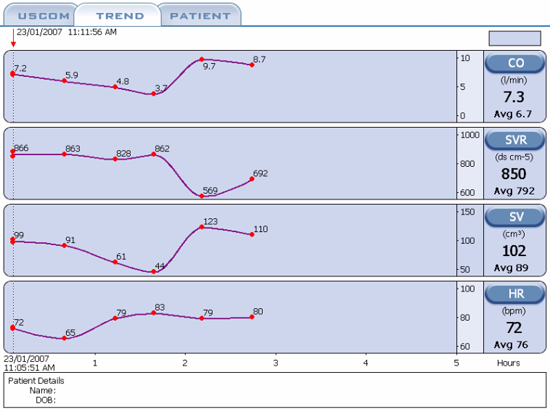
Throughout the procedure, which was carried out under a combination of general anaesthesia with IPPV and a thoracolumbar epidural, the blood pressure and pulse rate stayed within normal limits, whilst pulse oximetry and capnography were also normal. Just look at the changes in the hemodynamics shown in just these parameters! In particular, look at the readings for measurement points 3 and 5, at 1 hour 15 minutes and 2 hours 15 minutes respectively, where the pulse rate is exactly the same at 79. The pulse rate gave no indication whatever of the fact that the cardiac output and stroke volume had more than doubled, whilst the SVR had plummeted. The blood pressure also gave little indication of these profound changes.
The ease of using the USCOM in anaesthetized patients and the data that it provides, gives the anaesthetist a much clearer picture of just what his ministrations are actually doing to the patient, and also tells them exactly which way to go to correct the situation should a problem occur.
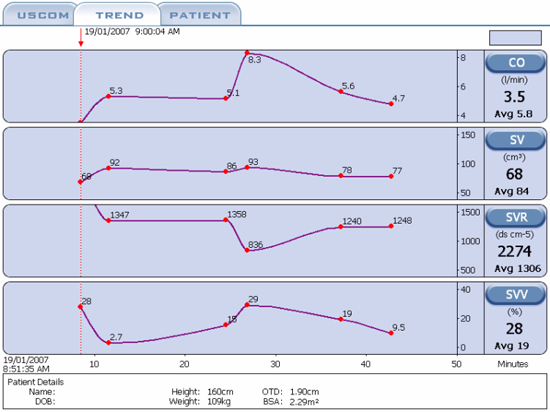
This second example is a 24 year-old female with pregnancy-induced hypertension undergoing caesarean section under a spinal anaesthetic. Due to the vasodilation which spinal anaesthesia produces, there can be marked falls in venous return with a consequent drop in stroke volume and cardiac output. As mentioned earlier, the drop in venous return can lead to a fall in myocardial contractility with reduction in the Vpk. In this situation, should we give fluid or should we use a vasopressor, and if so then how much? Should we use a combination of the two? If we use an excessive dose of vasopressor will this reduce the uterine blood flow with harmful effects on the baby?
About half-way through the case we see an abrupt fall in SVR and a sharp rise in cardiac output. Why was this? In fact this followed the administration of 10 units of syntocinon i.v. Syntocinon causes uterine contraction which we want to occur just after delivery, but it can also produce marked vasodilation. This patient had sufficient cardiac reserve to maintain her blood pressure by increasing her cardiac output significantly, but what if she had pre-existing heart disease and was not able to do this? In this situation we could give the syntocinon in small increments while monitoring her cardiovascular responses. Simple! The same applies to many other cardiovascular drugs in a host of patients. It is so much easier to make progress in small safe steps rather than try to redeem a situation which has already become desperate.
SVV and FTc.
This case also illustrates one other very useful feature of the USCOM which you see when you look at SVV, the stroke volume variation. This is often regarded as a very useful sign of cardiac preload. Although it has its limitations, in general, SVV increases as preload decreases. In a patient with a normal preload, SVV would be below 10% during spontaneous breathing and below 15% during mechanical ventilation at normal inflation pressures. Initially, following the vasodilation produced by the spinal block, the patient has a relative hypovolaemia, which shows as a high SVV. In response to rapid fluid administration, her SVV decreases to a more normal level. However, following the vasodilation produced by the syntocinon, we see an abrupt rise in SVV again indicating a relative hypovolaemia due to the vasodilation.
The USCOM also measures FTc, the corrected flow time. This is an indication of how long systole actually lasts, the correction being to enable different patients to be compared by adjusting the flow time to a nominal heart rate of 60 beats per minute, rather like the QTc of the ECG. If you think about it, the stroke volume that is ejected by the heart, taken together with the FTc, the time it takes to produce a stroke volume, must give a good indication of myocardial contractility. The more powerful the heart, the bigger the stroke volume (higher SV) the faster it will be ejected (higher Vpk) and the shorter the time needed for systole (shorter FTc). Many researchers have found that the FTc gives a better indication of left ventricular preload than does pulmonary capillary wedge pressure (PCWP or PAWP) or pulmonary artery diastolic pressure (PADP). The pairing of SVV and FTc are now regarded as a better index of total cardiac preload than the CVP and PCWP. The normal FTc ranges from around 325 in children to about 475 in older adults for the aorta and slightly longer at 325 – 500 for the pulmonary artery.
|