USCOM in the Out Patient Clinic.
No that’s not a misprint, the USCOM really does have major applications in the Out Patient Department and in the doctor’s office. Try this example.
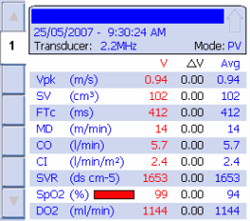
These are the hemodynamics of a 58 year old man with a history of hypertension. He is currently on atenolol 50mg daily, and has a BP of 155/95 and pulse of 56/minute. Would you increase his atenolol? Whilst you’re thinking about that, what if I told you that he is complaining bitterly that “I just don’t have any energy to do anything. I’m falling asleep all the time. I never used to have that problem”? The USCOM tells us exactly why this man is not happy. His cardiac output is depressed to the point that he would almost qualify as chronic heart failure, the lower limit of CI being 2.4 l/min/m2. His SVR at over 1600 tells us where the problem lies. If we start from BP = CO x SVR then there can only be two causes of hypertension, either the CO is too high or the SVR is too high. (Very rarely, both are too high.)
In this case the way to treat the raised BP is surely with an agent that reduces the SVR. This could be an ACE inhibitor, ARB, calcium antagonist or whatever. By lowering the SVR the BP will fall, even though there will also be an increase in cardiac output once the afterload has been reduced. The increased CO will help his symptoms of lack of energy. Ultimately, he might require a combination of agents. Time and the USCOM will tell, but there is no need for guesswork anymore.
So now you might be thinking that vasodilators such as ACE inhibitors and angiotensin receptor blockers are the way to go in hypertension. Well try this patient.
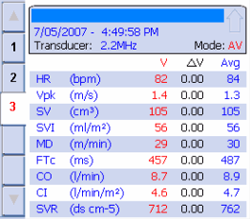
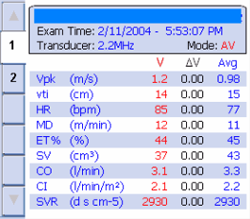
This 88 year old lady is normally very fit and well, but has been to see her doctor several times in the last two months complaining of tight chest pains, breathlessness on exertion and dizziness on standing or coughing. She claimed that she had been “just fine until they changed my blood pressure tablets”. What does the USCOM show? Can you guess what type of medication she is on for her hypertension? What does the USCOM data suggest that we should do to treat this patient?
O.K. so ACE inhibitors and ARB’s aren’t the be-all and end-all of hypertension. There are horses for courses. ß-blockers have their place, as in this case. Some patients are better on a thiazide, some on ß-blockers, some on ACE inhibitors, some on calcium antagonists or whatever. Some do better with combinations of agents depending on their hemodynamics. What is abundantly clear is that claims by pharmaceutical companies that their drug is the answer to hypertension are patent nonsense, if you pardon the pun. With the USCOM, we can not only see which way to go for the best, but we can easily spot adverse effects of our treatment. Perhaps it’s not too strong to say that the days when we treated hypertension by just measuring the blood pressure are gone. As for prescribing on the basis of the drug written on the side of the “free” ball-point pen or other advertising gimmicks, don’t you think we owe our patients rather more?
Chronic Heart Failure.
This is one of the commonest conditions seen in Medical Out-Patients or in doctor’s offices. There are literally millions of patients treated every day with combinations of drugs for chronic heart failure. Digoxin, diuretics, ACE inhibitors, nitrates and ß-blockers are all prescribed to patients daily, yet how many patients have their cardiac output measured or even reliably estimated? How do we gauge the effectiveness of our therapy? In the main, this consists of asking the patient if they feel better or can do more. It is at best highly subjective. It would be inconceivable to treat hypertension without measuring the blood pressure, so why do we treat heart failure without measuring the cardiac output? Until recently the answer would be “because we can’t measure cardiac output”. Well not any more. We now have a simple and accurate tool for doing what we have all wanted to do for years, so let’s get to it!
This 63 year old woman has a history of breathlessness, orthopnoea, palpitations on exertion and tiredness. She has pitting oedema of the feet, ankles and lower calves. What do you see in her hemodynamics? Her medication at present consists of digoxin 0.125mg daily and frusemide 40mg daily. What medication changes would you consider here? What would you like her readings to be after you have modified her therapy?
The USCOM not only makes the diagnosis easy (not that this one is difficult!) but quantifies the problem. It shows us that the afterload is the main issue that we need to address, it almost tells us which drugs to use, and then gives us our therapeutic targets. Goal directed therapy as it should be. But best of all, after the change of therapy, we can re-measure the hemodynamics and make sure that we are helping the problem primarily, but then we can go on to optimise therapy. Why settle for “better” when you can have “best”?
|