Section A - Hypodynamic Circulation.
Now using the USCOM we can identify more exactly where the problem lies. Why is the MD low (<14m/minute)?
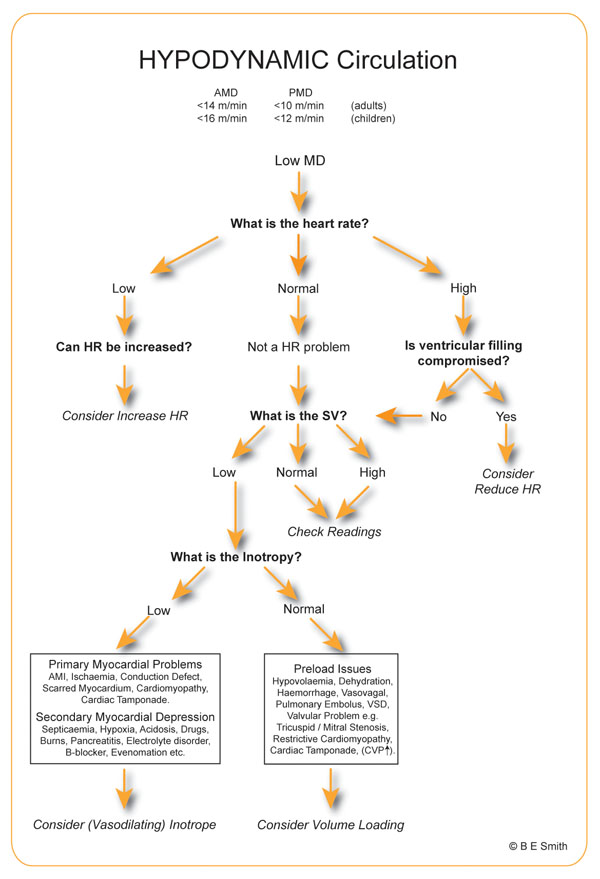
In this way the hypodynamic circulation can be reduced to just two problems – assuming HR is not the problem –
1. Insufficient preload or ventricular filling,
2. Pump Failure.
Hypodynamic circulation means we should be looking at the circulation before the aortic valve. A hyperdynamic circulation is very different as we will see in section C.
Hypertension.
There is one very important exception to this rule; hypertension due to a high SVR - vasogenic hypertension. As BP = CO x SVR, hypertension can be caused by either a high CO, a high SVR or a combination of the two. If the SVR is high, then the heart may be unable to maintain a normal CO against the high afterload and the MD will consequently fall. On the other hand, in cardiogenic hypertension the high CO will lead to an increased MD. Again, MD gives us an instant reference value to identify the cause of the hypertension. We can then confirm and quantify the problem from the USCOM values.
Inotropy.
This also shows the importance of inotropy measurement in making sense of a reduced SV. The SV could be low because the preload is low, the afterload is very high or it could be due to low cardiac inotropy. If the SVR is over 1600 then we have an afterload issue. If the FTc, SVV and LVEDVI all suggest that the preloading is OK but the Smith-Madigan Inotropy Index (SMII) is only 0.9W/m2, then we are looking at cardiac failure. The decision to use an inotrope then becomes very easy.
On the other hand if the SMII is 1.4 W/m2 and the FTc and LVEDVI look to be low whilst the SVV is high, then this is almost certainly a preload problem. A passive leg lift test should clarify the position. (See booklet 3 “The USCOM and Inotropy” for the details of the passive leg lift test.)
However, you might say that an SMII of 1.4 W/m2 is a bit low. Yes it is, but inotropy responds to preload, so if we increase ventricular filling then we stretch the cardiac muscle fibres a little more which increases the force of contraction, as Starling explained. If preload is low then ventricular stretching, and consequently inotropy is reduced. A slightly low SMII is therefore typical in low preload states. We see a similar situation in cardiac tamponade where the ventricle is not allowed to fill properly and the cardiac myofibrils are not pre-stretched. Not only will SV be low, but so too will be SMII, and may be very low (<1.0W/m2) in symptomatic patients.
So a hypodynamic circulation that is not due to either a tachyarrythmia or bradycardia either needs preload increase, afterload reduction or an increased inotropy, or a combination of these. Now, that makes sense!
Take a look at the data below. The MD is just 10 m/min; a hypodynamic circulation. Can you explain why this is, and also how to treat this 57 year old 76 Kg male patient? His BP is 106/64 (MAP - 76mmHg).
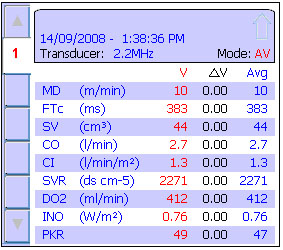
The MD is low, the SV is low, CO and CI are low. His DO2 is also low, we would expect around 12–15 ml/kg/min or around 912–1,140 ml/minute in this patient. The FTc at 383 is about normal which suggests that this is not a preload issue. The SVR is high, which could be primary or could be secondary to the low CO, i.e. he is vasoconstricting to try to maintain blood pressure. Given that his MAP is just 76mmHg, this doesn’t look much like vasogenic hypertension! The SVR must therefore be secondary compensation for the low CO. The SMII (or “INO” on the USCOM screen) is only 0.76 W/m2. This is typical of myocardial failure, which was treated with dobutamine, to increase the SMII and CO and lower the SVR! Now that was easy!
But there’s more. We said his DO2 needs to be increased to around 1,000 ml/minute. His cardiac index is only 1.3 l/min/m2. If we doubled his CO to a more normal level (a CI of 2.6 l/min/m2) his DO2 would only increase to 824 ml/minute. There must be something else going on.
Now we know that DO2 = 1.34 x Hb x CO x SaO2% so either this man has a low haemoglobin (Hb) or a low SaO2. So which is more likely? If you are using an Oxycom (USCOM with built in pulse oximetry) then the answer is obvious. His SpO2 was only 84%. Increasing his CI to 2.6 l/min/m2 and his SpO2 to 100% would give us a DO2 of about 980 ml/minute – close enough!
Sometimes the initial USCOM values might be on the edge of normal. It is always worth reviewing these in more detail. You’d be surprised what this may reveal. Below are the initial USCOM measures from a 47 years old male weighing 89kg with a BP of 144/86 (MAP-105mmHg). He complains “I just have no energy and I’m always tired”.
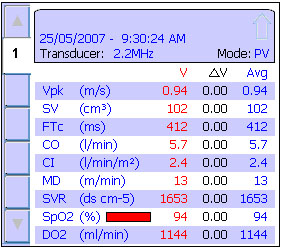
If you follow the algorithm then you’ll see that this man is borderline hypodynamic. The next question according to the algorithm is “What is the heart rate?” You haven’t been given this, but you can work it out from his SV and CO (5,700ml/102ml). In fact it is 56/minute. Does that give you any clues? His SVR is rather high for a man of his age and his SpO2, measured from a finger probe, is apparently low at just 94%. Got it yet?
Well something is giving him a bradycardia, is increasing his SVR and maybe giving him vasoconstricted fingers as well. You know his BP is elevated. Could this be iatrogenic? The answer is yes, he’s being treated with the β blocker drug atenolol. His CI is right on the edge of cardiac failure which is why he feels tired. But what can be done about it?
He clearly needs an increase in his CO, but if his SVR were to stay at 1650 the increase in his CO would also increase his BP. Therefore his SVR needs to be reduced and his CO increased at the same time, thereby reducing his BP from the current level of 144/86. The answer of course is to switch him over from atenolol to a peripheral vasodilator.
This patient was slowly withdrawn from atenolol and commenced on an ACE inhibitor. His BP reduced to 132/76 (MAP-95mmHg), his pulse increased to 74/minute and his CI rose to 3.2 l/min/m2. His SVR fell to 1124. More importantly he reported feeling “better than I’ve felt for ages!” Well, that’s no big surprise when you understand the haemodynamics!
On the other hand, this 68 year old female of 63Kg was being treated as an outpatient for chronic heart failure. Are there any pieces of the jigsaw that you feel are missing? What other indices would help you to understand this?
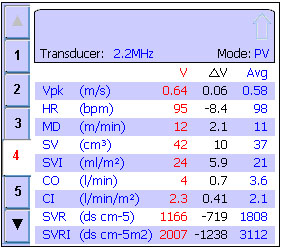
If you answered “what is the SMII and what is her FTc” then you’re ready to move on to the next section, but before we do you might just like to see what her cardiac index had been doing over the previous 8 weeks that she had been coming to the hospital....
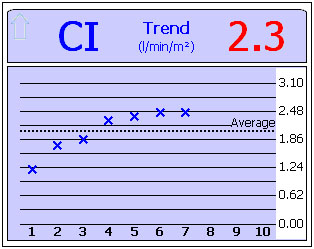
A CI of 2.46 might not seem that great, but it is significantly better than the 1.22 L/min/m2 of her initial presentation; a 101% improvement in CI! Reading 2 was taken after she started a diuretic, reading 3 after she commenced on digoxin, and reading 4 after an ACE inhibitor was added. Logical therapy without guesswork. |